click here for pdf English
Weekly Update on COVID19 situation
JAN SWASTHYA ABHIYAN (JSA) AND ALL INDIA PEOPLE’S SCIENCE NETWORK (AIPSN)
Dated 2nd April, 2020
- Making Sense of the numbers:: Where are we in the epidemic curve
- The lock-down and its sheer brutality
- Do lock-downs work?
- Health system preparedness
- The peoples movement response
Part I. Making Sense of the Numbers
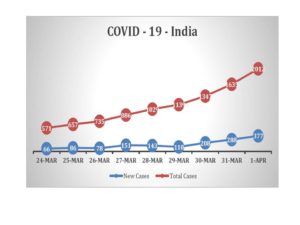
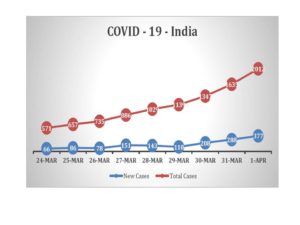
In India the COVID19 epidemic has reached the 64th day since the first case was reported on January 29th. The number of cases crossed the 100 cases mark three weeks back, on March 14th. At the start of the lockdown India was at 648 cases, which doubled (close to 1251 cases) within six days. .
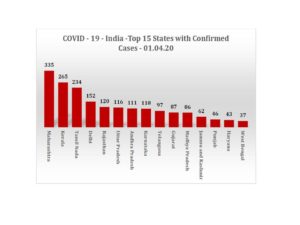
As of 1st April the total COVID 19 positive cases are 2012. The growth rate since 24rd March is 252% and the daily growth rate from 31st Mar to 1st Apr is 23% (see chart below).
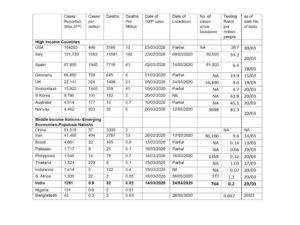
Globally there are now 801,064 cases which translates into an average of 102 COVID positive cases per million population. The total deaths reported are 37,815, which works out to a mortality rate of 5 per million population.
India in contrast has a case rate of only 0.9 million per million population and a death rate of 0.02 per million. Does this mean that we are doing well for this stage of the epidemic, or is it too early to tell? To analyze this, our weekly update looks at cross country comparisons, our testing protocol and case definitions and the entire narrative on ‘stages of the epidemic’.
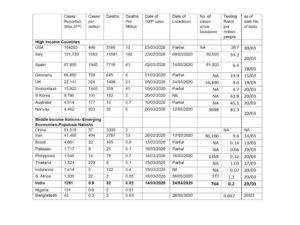
Table : Cross-Country Comparisons
Sources:
- Data for USA testing rates is from https://covidtracking.com
- Data for testing rates for India, Bangladesh and Pakistan is from Wikipedia
- Data for testing rates for all other countries is from https://ourworldindata.org/covidtesting
- Data for dates of 100th case and number of cases since lockdown is from https://coronavirus.jhu.edu/map.html
- Cross Country Comparisons:
While the first case in most nations occurred at about the same time,- but as the table above shows, there has since been a big divergence between the experience of the high income countries (HIC) and a selection of relatively high population low or middle income emerging economies (LMICs) (https://www.worldometers.info/coronavirus/#countries)
Between these two groups, the divergence in both incidence and mortality is huge. High-income nations appear to have a much higher infection rate and even a much higher mortality rate. Iran and Thailand are outliers in the middle-income countries group since they have relatively higher infection rates. But they are also known to have more universalized health care systems.
Within the high-income nations too the experience can be very different. But on the whole they have much higher infection rates than the LMICs irrespective of the date of first infection or the date of lock-down. One probable reason is the testing protocol followed (whether mild and moderate cases or all asymptomatic cases are tested) and the capacity to deliver these services, both in terms of test kit availability and access to testing. The more one tests, the more one uncovers positive cases. The alternative to such an explanation is to believe that LMICs on the whole have a higher resistance to the spread of infection. But that does not seem to protect nations like Thailand and Iran who are known for both better health systems and better health sovereignty.
Absolute Mortality rates is a true reflection of the health burden imposed by the disease and here there is a clear difference between the different nations. Case Fatality rates are important, but at this point of time could be misleading. We need to adjust for testing rates and protocols. They could be appearing high in Italy and Spain, and certainly in UK because tests were not offered to many of those with mild or moderate symptoms, whereas in South Korea it may appear low since more persons were tested. We will know for sure only later, when studies measure the total proportion of those who were infected- and calculate the proportion that were asymptomatic, mild or moderately symptomatic, and the proportion with severe symptoms, and fatality.
That being said- after adjusting for testing rates we find that some countries such as US, UK and Belgium have a much higher proportion of positive cases and others like South Korea and Australia have lower positivity rates.
Moreover, even for a certain level of incidence- certain countries like Germany, Scandinavian countries, Japan and South Korea had much less mortality. What we can conclude: One can comment on true incidence of COVID 19 only when testing rates conform to a protocol where ideally a) all symptomatic cases are tested and b) all asymptomatic contacts of COVID 19 positive cases are tested. If the testing protocol fails to test the above, the incidence rates must be adjusted accordingly by modeling or computation, assuming that the proportion between asymptomatic, mild, moderate and severe is the same universally. Similar adjustment is required for commenting on mortality too. However, in nations where accurate cause of death reporting is universal, such as in most HICs and countries like Thailand, absolute mortality rates would also be indicative. However this is not the case in India and the increment mortality that COVID19 may cause, may not be readily visible.
- Comparisons between states:
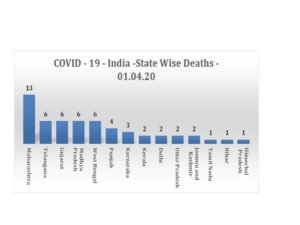
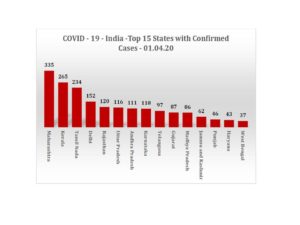
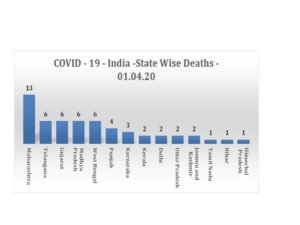
The following charts show the number of COVID-19 infections and related deaths across 15 States with the highest numbers (See charts below). Maharashtra has the highest number of infections and deaths.
- Testing Protocols in India:
The current testing protocol in India could seriously under-estimate the number of COVID 19 positive patients in India by about 80%. India has allowed testing only for severe acute respiratory infections where a) the age is over 15 years there is fever and one respiratory symptom- cough and shortness of breath AND requires hospitalization; b) OR has traveled abroad c) OR been in contact with a confirmed case of COVID-19 positive case in last 14 days, d) OR any health worker admitted with severe acute respiratory infections (SARI).
Further, it also stipulates that if the history of travel and contact is not there, then only half of those admitted patients would be tested. While this may be good enough for a research study, the hospitalized half not tested actually has an equal chance of having COVID 19 and therefore could infect the entire staff and patient attendees. Further, if there is no increased number of cases- and there is just the same number of cases as was already there in the previous 15 days, no one however serious and typical of COVID19 infection, needs to be tested.
Informally and anecdotally, reports from across the states indicate difficulties in getting it tested even where ICU mortalities have occurred. There is almost an unwritten order within the system to keep the numbers low.
- Case Definitions in India:
Current case definitions in use for mild or moderate case of COVID 19 need to be examined. The WHO case definition of a mild case is: “Patients with uncomplicated upper respiratory tract viral infection, who may have non-specific symptoms such as fever, fatigue, cough (with or without sputum production), anorexia, malaise, muscle pain, sore throat, dyspnea, nasal congestion, or headache. Rarely, patients may also present with diarrhoea, nausea and vomiting (3, 11-13)”. The Public Health England definition is even wider. In India however, the case definition emphasizes fever AND cough AND shortness of breath. If there was only fever with sore throat and limited cough or nasal congestion this would not even be considered as suspect.
When by definition all mild and moderate cases are excluded from testing, – we should then assume that prima facie over 80% of all COVID 19 cases will not be picked up and interpret our figures with that important caveat. Our numbers are therefore well designed under-estimates.
- ‘Stages’ of the Epidemic in India- an ICMR innovation?
In India, ICMR has created a narrative built around epidemic stages, which is widely adopted by the media and now also by very many reputed clinicians who are briefing the media. Indeed, this was first announced in a well-attended media briefing.
The narrative goes like this: India is at stage 2 of the epidemic and this is a manageable stage. A lock-down is meant to prevent it from going to stage 3, which is a terrible stage to be in, where we lose all control and an irreversible and terrible situation has set in. Thanks to our lock-down we are remaining in stage 2 and have been saved from stage 3. Stage 2 is characterized by the fact that we can trace back every case to a case of international travel. This is therefore called local transmission. Whereas in stage 3 we cannot do so- and therefore will be called community transmission.
There are many problems with this narrative. Firstly, WHO does not use such stages nor are we aware of such stages in any major public health texts. WHO does talk of four phases- the third being amplification and fourth reduced transmission- but containment, control and mitigation are overlapping concepts.
Secondly, though local transmission traceable back to an international travel contact is important and may be the exclusive form of case identification in an early stage of the epidemic, it has no relevance at this level of disease incidence. We know that a large number of travelers have entered in whom symptoms develop late, or they were from nations, which were then not known to have transmission. Further there are very many asymptomatic carriers of the disease who will never even know they have it and therefore transmission without a known contact is happening. Indeed such transmission is widely reported, but the government is not willing to give up its narrative, and ad hoc explanations appear- “oh this is only a small minority of patients”, or “we are still tracing the contacts”. That is not the meaning of the term “community transmission”. Further, whether a contact is identifiable or not is also dependent on subjective factors like patient recall, or skill in contact tracing. And then most importantly, we do not allow for testing anyone without contact history- therefore creating by design an absence of evidence to detect community transmission and then touting such data as the evidence for its absence.
Finally there is no big break-point between these two stages. Stage 3 is just as reversible as stage 2 and stage 2 just as likely to continue to generate cases. What matters is the rate of increase of incidence of infection, and if it is increasing exponentially, the action that is required. At this moment we cannot predict in whom the fresh cases are likely to occur, and instead we are tracing back to find out from where they got it. Whereas, we have already reached the stage where the main strategy should be identify all likely cases, isolate, test, treat and trace their contacts for further testing and isolation.
The probable reasons why the narrative of ‘stages’ is being maintained could be the sense of triumph in the declaration of still being in stage 2 and the sense of horror created by the threat of entering stage 3 are necessary to justify and manufacture the consent that is required for this brutal lockdown in India. We could live with this, except for the fact, that maintenance of this false, misleading and irrelevant epidemic stages, leads us to justifying the exclusion of mild and moderate cases from testing and well planned isolation. This is also leading to a huge amount of victim blaming when each instance of the disease can be traced back to some transgressor- where the accountability of the government is only in not being authoritarian enough. Recently this has also taken a communal turn. Governments filing FIRs or taking other action against such offenders follow this, with a large section of media applauding it. On closer examination most such charges are without merit.
Further, these mild and moderate cases are being handled in our regular outpatients as non-COVID ARIs and even 50% or more of our severe and hospitalized COVID 90 patients are being examined and treated by healthcare providers without any personal protective equipment (PPE) whatsoever. Recognizing this, the government has made all symptomatic healthcare workers eligible for testing and further allowed an as yet under-investigation drug Hydroxychloroquine for chemo-prophylaxis- but this is not quite the way to go.
The call from people’s movements to the government is to drop this narrative of stage 2 and stage 3, and instead talk of immediately initiating the isolate, test, treat and trace- as the main strategy in readiness for the lifting of lock-down on April 14th. The lockdown has bought the system valuable time to prepare for the epidemic and was to some extent inevitable due to the weight of scientific opinion as was available then to the government, but now that we have the experience, and also understand the collateral damage it causes we could review this strategy and learn the lessons so that we do not have to repeat this in the future. We should also stop misleading comparisons we make with European nations which have different contexts and note that our figures are more comparable to much of Africa and the more economically and socially disadvantaged countries of every region.
Part 2. The Lock-Down and its brutality
The other major feature of this week was the lock-down. In sheer scale and scope few nations have seen anything like this. The program theory that justifies lock-down is that the measure of the contagiousness of a disease is dependent, not only on the virulence of the organism which we can do nothing about, but also to the number of contacts between an infected person and a non-infected person. It is an extreme and enforced form of physical distancing.
The lock-down was anticipated to cause economic slow-down, and personal hardships and some curbs on individual rights, but the rationale was that this was the price the country and its people had to pay for safeguarding us from losing anywhere from an estimated 0.5 % to 3 % of our population which could be many millions and if we go by the lower estimates it would still be thousands of deaths.
As expected, the lock-down did cause hardships to all- but very disproportionately. When the lockdown was introduced the hardships presented in the media either related to corporate concerns like economic slowdown, or middle class concerns like inability to buy groceries, boredom, managing with maid-servants etc. In hindsight it appears that there was absolutely no recognition or consideration in policy circles of who the majority of the country were and the conditions of their life. There was neither planning nor messaging related to problems like farmers having standing crops ready for harvest, or fishermen who could not go to sea, or the millions of daily waged migrant labour who live on the brink with no social security whatsoever. The immense tragedy that has followed, in terms of mass migration and hunger, was clearly unanticipated by government. It made clear the real social distance between the ruling elite and the majority of the people. It also made a mockery of the efforts at physical distancing. The large movement of people after the lockdown means that the key objective of the lockdown failed and has in effect rendered it as ineffective. The lockdown has created conditions suitable to transmission of COVID-19 infection. Moreover, the number of deaths due to such distress, hunger, lack of transportation and lack of access to healthcare for other diseases, may in fact be many times more than the deaths due to Covid-19 infections.
The social, economic and human cost being paid by the poor is enormous. Relief measures were not announced in parallel with the lockdown announcement. Two days later the government announced a very incomplete and inadequate package of measures that could not win the confidence of the people or stem the huge surge of migration all across the country, as fearful working people made a desperate bid to get home. Instead of responding with utmost sympathy to this distress migration, and strengthening relief measures, the government response was brutal, insensitive and at the end of the day- ineffective as well.
There are many contenders for the most shameful of the orders passed or measures enacted to prevent this migration and to enforce the lock-down. One example that shocked the nation was that of a group of migrant workers being sprayed with chemicals. Another is the Haryana government order creating temporary jails and calling for the arrest of migrant families walking on the road with luggage and young children as “jaywalkers.” In a series of press releases and public statements the peoples health movements have protested such brutalities and unethical behavior of the state and of communities. (See JSA-AIPSN statement on state obligations during the lock down (http://phmindia.org/2020/03/29/government-responsibilities-during-lockdown/ ) and JSA-AIPSN press release protesting criminalization and use of coercion and violence against the movement of migrants (http://phmindia.org/2020/03/31/press-release-retract-notifications-that-criminalize-use-coercion-against-the-movement-of-migrants/) )
The fear and victim-blaming that was rampant in all official messaging on the epidemic has also led to a huge degree of stigmatization and hatred within communities. One form, which it took, was doctors and nurses engaged in the struggle being thrown out of homes and refused entry into residential areas, as fearful residential colonies locked-down. Another was the hostility shown to those on whose houses quarantine notices had been stuck. Such public naming and implicit shaming and measures like public circulation of names of those who had been on international travel and of COVID patients- all in sheer violation of all ethics related to privacy and confidentiality- did not help the cause of physical distancing (See JSA_AIPSN statement protesting breach of confidentiality and privacy (http://phmindia.org/2020/03/23/jsa-statement-on-breach-of-confidentiality-around-coronavirus-cases/ ) and JSA-AIPSN statement regarding concerns on isolation and quarantines (http://phmindia.org/2020/03/24/jsa-statement-on-concerns-with-regard-to-isolation-and-quarantine-covid-19/ ) ). Clearly the perpetrating authorities were unaware of centuries of public health experience in epidemic management that teaches us how fear and stigmatization lead to families hiding the episodes or illness and circumventing rather than following the requirements of quarantine and physical distancing.
It was not only the migrant workers who were affected but all working people- especially farmers, agricultural labour, fisher folk, tribals, construction workers, sex workers and other unorganized sector workers. The relief measures were often a re-packaging of items already on the budget or very small tokens of relief. The JSA-AIPSN has brought out a statement explaining the inadequacy of the proposed measures at economic mitigation and articulating people’s demands for relief and mitigation (See JSA_AIPSN statement on the economic package announced by FM with respect to COVID19 pandemic and the lockdown (http://phmindia.org/2020/04/02/statement-on-the-economic-package-announced-by-fm-with-respect-to-covid19-pandemic-and-the-lockdown/ ) ).
One important component of this litigation is the urgency to prevent hunger and starvation. The Right to Food Coalition has issued a statement in this regard (Right to Food Campaign- statement on urgent Steps for Mitigation of Impact of Covid-19 on the Poor and Vulnerable during the lock down and coronavirus pandemic (http://phmindia.org/2020/03/20/letter-to-the-pm-demanding-for-urgent-steps-for-mitigation-of-impact-of-covid-19-on-the-poor-and-vulnerable/ ) ). Another important component was the way the lock-down hurt access to essential healthcare services. Partly this was due to lack of transport, but in part because essential health services were shut down or diverted to make way for services to address the epidemic.
The JSA has documented the crisis in access to essential health services due to the lockdown and written to the government demanding that such services must be continued through this period, with special arrangements made for the sick to access services during this period (See JSA-AIPSN statement on lockdown and suspension of essential healthcare services (http://phmindia.org/2020/03/27/statement-against-closing-essential-health-services-during-lockdown/) ).
We also note that among working people themselves and in civil society there are also outstanding individuals and organizations who have come out, sometimes at great risk to themselves to help those in such great distress. These have to be built on- but cannot substitute for the obligations of the government under a lock-down. Individuals have obligations which most follow to the extent it is feasible for them- but the big question we ask is whether the government is able to fulfill its obligations. The JSA and AIPSN have released a number of statements that highlight the consequences of the lock-down and immediate action that government must take to ameliorate this crisis.
Part 3. Do lock-downs work?
One of the big questions that have arisen is whether lock-downs work. Firstly it must be noted that much of the scientific justification for lock-downs lies in a combination of mathematical modeling and the assumptions it makes as well as expert opinion. There is very little hard evidence. The problems with the models are many.
Most models never factored in the social costs and collateral economic damage and reduced access to health care. None of the models even attempted to model for equity and the differential impact that a lock-down would have on different sections of society in different nations. The working people in a nation where most of the workforce is in the organized sector, where universal healthcare is a reality and where social security covers all sections like the North European and Scandinavian nations, is clearly less likely to suffer such damage as compared to a nation like India, where most of the workforce is in the unorganized sector progress towards universal health care is minimal and where for the vast majority there is no social security. It is not only economic outcomes one is worried about- it is also health outcomes. Of course most of the increased mortality that would result from the lock-down will be on the poor, whereas at this stage of the epidemic, arising as it is from international travel and their contacts a major part of the morbidity would be on the more affluent. Had all of this been factored in, the least the experts could have done, was to give a week time for people to get home and better arrangements to be made. The logic of announcement of demonetization or an enemy strike is one thing, but the logic of shutting down all of people’s social and economic life is quite another.
Models also never factored in how the epidemic plays out in different context of immunity, vulnerability and virulence. They also did not factor in what would have happened in scenarios where the lock-down was more focused on hotspots and vulnerable sub-sections like age, and the identification of these hotspots guided by testing. Finally, the reasoning for the lock-downs has not quite figured out what happens after a lock down is lifted, the number of days the infection will take to reach back to the same level of spread as now.
On the other hand there is clearly one major benefit of the lock-down that there is a consensus on- that it flattens the curve- i.e. delays the peak of the epidemic and prevents a huge surge of cases giving time for health systems to prepare themselves. Even on this, we need to keep an open mind- since in practice the level of physical distancing achieved may be negligible because of the problems of implementation and because preparation in such short times is really not feasible. If South Korea and Japan and Germany have done better, these were precisely the three nations who had the technological capacity to scale up testing based on indigenous capacity plus also had the highest bed to population ratios and ICU bed to population ratios even within the developed world.
The best time to have started preparation was actually at least 15 years back- but failing that, the next best time would be now.
Given these very many uncertainties about the benefits of a lock-down and the very certain ill-effects the least we can do is to measure its effectiveness and in a gradual and phased manner, starting now, lift the lock-down and make arrangements so that it is not needed again after 14th April.
Part 4. Health system preparedness:
Irrespective of its narrative on stage of the disease or the effectiveness, health system preparedness to meet this pandemic is essential.
We note that there are several major very welcome developments in this area- and we list these below:
- The finance minister announced a fund of Rs 15,000 crore to strengthen the health systems to meet this challenge. This was much needed. Such an amount should anyways have been part of the annual budget, in fulfillment of the government’s own policy commitments to the health sector. But given the fact, that this is coming after years of under-financing, it would be inadequate to close the gaps. Further, much of the strengthening of health services- whether it is by hiring more human resources or by increasing ICU beds and ventilators cannot and should not be seen as a transient measure. What would have helped and could still help the state governments in utilizing this amount effectively, is a clear commitment by MOHFW to retain this amount in future budgets as well.
- The government has sanctioned three companies last week for production of test kits for COVID2. These three promise to reach a capacity of about 30,000 kits per day. Another 11 companies were in the queue for approval, and by now are probably approved. But some of these are importers and importing now may be impossible. The government aim is to reach a testing capacity of 60,000 per week, which may seem a big target now, but in practice is still too low. The way forward would be for the government to support private companies with both financial resources and imported technical support (perhaps from the South Koreans) to accelerate indigenous production to close to 1 lakh per day, and bring the costs down to Rs 300 per kit or less. With the availability of kits, hopefully the protocols for testing would be changed. However by the time of the lockdown we may reach only about 30,000 kits per day. As we go to release this we have disturbing news of a crisis in the availability of reagents. Though the government action on this has been very delayed, it is welcome, There are many concerns regarding the impending severe shortage of APIs for essential drugs, issues of Intellectual Property Rights related to new drugs , medical kits and vaccines and on the government’s approach that the JSA, AIPSN and AIDAN have written to the government about (See JSA-AIDAN_AIPSN letter to prime minister on scaling up access to free testing and treatment for COVID 19 (http://phmindia.org/2020/03/25/letter-to-the-pm-addressing-issues-of-scaling-up-access-to-free-testing-and-treatment-for-covid19/ ))
- The government has passed an order stopping the export of ventilators in the second week of March. Further it has placed an order for 10,000 ventilators to become available before mid-April and another 30,000 to become available in one more month. The government has taken note of some private hospitals to buy and hoard ventilators and of private companies to sell at higher prices to them. Ventilators must be now declared an essential commodity, and government should ensure proper allocation and deployment of these as and when they become ready. We note that 40,000 ventilators in a month is optimistic, especially when the orders are yet to be finalized, but here the government is on right track.
- The government has identified a number of sites in larger cities; largely student hostels, guest houses, and sports facilities, which it can use for quarantine and potentially for isolation of COVID 19 patients who do not need hospitalization. We have no clear information about how many such student hostels and sports facilities have been so requisitioned.
- The government has also identified one or two hospitals for each cluster of districts that can be brought under a public authority for exclusive use in management of COVID 19 severe cases and critical care. In some large hospitals it has identified wards and/or sections of the hospital for such use.
- The government passed an order stopping export of personal protective equipment (PPE) in early February. Since then it has placed an order, including emergency imports for PPE through the government owned company HLL Lifecare limited. It is also in the process of giving sanction to Indian manufacturers of the same. Though these are steps in the right direction, we have concerns about the adequacy of these arrangements, on which we have written to the government. This could be another major bottle-neck. This could also be contributing to the pressures to identify less number of cases. The JSA-AIPSN will be writing to the government in this regard.
- There are many areas where many states are not making enough efforts. Only one or two states have made moves to address the gaps in ambulances and patient transport systems that would be needed. Many states have large gaps in human resources and in supply chain management systems that they are not addressing. Training is also behind schedule in most states. Most states have also not begun efforts to prevent hospital acquired COVID19 infections. The JSA-AIPSN has written to the government on many of these gaps in health system strengthening and what corrective actions that states must undertake as a priority (See JSA-AIPSN letter to government on health system preparedness (http://phmindia.org/2020/04/03/letter-to-secretary-health-which-encloses-our-statement-on-health-systems-preparedness/ )). We are also monitoring the efforts to rapidly build up health systems and collecting more details on ongoing health system preparedness as happening in the states.
- In conclusion, though in denial of the extent of spread and very delayed and inadequate in scale in preparedness, this last week has seen a series of policy initiatives that address most requirements for health systems preparedness, backed by the funds needed to achieve this. There is also rise in seriousness across states though some states are still slow to begin, or focused on only one or two dimensions of preparedness. An useful collation of orders by state governments (including state Health Departments) is being updated and made available here covid-india.in
- One priority area where the plans of the government are not clear or consistent is the strategy for mild and moderate case who could be as much as 20 to 30% of the entire population. Even if we assume that these patients are in homes due to the lock-down, as soon as lock-down lifts, those they have infected would be moving freely in the population- and their family members and primary healthcare givers would be unaware and unprotected. This would be a major source for spread of the infection. Our suggestion is that there must be an intensive effort, with help of community and voluntary team to identify all those with mild and moderate symptoms, test them for the disease, and if positive offer institutional isolation to them. Only if they are in a position to practice home isolation effectively or if in that district it is not possible to arrange institutional isolation should home isolation be preferred. For such a strategy there is are two requirements- (a) expand access to testing, and where possible try to organize sample collection from home in response to a call to a help-line call (with all necessary safety precautions) or for patient transport to designated sample collection centre. And (b) identify a large number of spaces that could be considered for institutional isolation and plan the systems required to set these up and manage them when the need arises. If the government is not ready to undertake this, we must understand that the government is opting for a strategy where the majority get infected and recover, giving rise to herd immunity, while government only takes care of the very sick. But if that is the plan then such a huge all out lock-down should not be resorted to.
- We are also concerned about some recent reports of strategies of containment that have no basis in evidence or the science of public health. One such innovation is to define a 5 km radius around a COVID-19 hotspot as a danger zone and a further 3 km as buffer zone and lock down everyone within these zones as well as universal masks etc. This appears like another whacko modeling effort gone wrong, where physical distance is being interpreted literally and not along the lines of a social distance defined by the economic activity and production and social relationships in that area. When efforts are made at modeling, there is an urgent need to see that there are social scientists and public health expertise as part of the team.
- One area where innovation would help is point of care diagnostics to identify those who are immune to the disease and no longer infective- for these would make much more effective volunteers, requiring less protection and be able to serve in the different frontlines. If the epidemic plays out as per current projections the government is going to require a large number of volunteers.
Part 5. The Response from Peoples Movements and Communities:
- This week has also seen the build-up on a major response across people’s health movements, people’s science movements, women’s organizations, trade unions and associations of working people, civil society organizations and community based organizations. These organizations have also sought and got support from a number of progressive intellectuals and scientists and public health experts.
- The JSA and the AIPSN have been holding consultation on Skype and have tried to understand the developments, critically review and in consultation with domain experts brought out a number of papers and statements that can inform their own membership and the general public. They have also articulated demands for better COVID 19 control and for better mitigation of the social and economic costs of the lock down through a charter of demands and a number of press releases and petitions to the government.
- In addition to these statement, the JSA and AIPSN have launched campaigns to inform its own members and the general public of the dangers from this epidemic, how to keep the community, themselves and the public safe and to counter fake news, stigmatization and victim blaming messages that emanate both from sections of the government and communities. (See PHM Advisory for Families and Communities, and PHM FAQs on the COVID 19 pandemic (http://phmindia.org/2020/03/28/advisory-for-workers-cleaning-hands-in-low-resource-settings-and-protection-in-crowded-places/ ). There are also short videos and WhatsApp posters that are available.)
- Because of the lock down, extensive field level mobilization and community support action has not been possible, though in many states, organization who are part of this network are engaged in organizing community kitchens. Once the lockdown lifts, a major effort at social bonding and mobilization to counter hate campaigns, and provide support to affected families and communities, is being planned.
- We would be sending this weekly update along with a special press release that would a) demand a review of the lockdown and an phased withdrawal of the same; b) an acceleration of work in preparing the health systems for the epidemic through a more comprehensive approach and c) a call for much more participatory and less authoritarian approach to controlling and mitigating this pandemic.
For further information, please contact:
T.Sundararaman – 9987438253
D.Raghunandan – 9810098621
Sarojini N. – 9818664634
Sulakshana Nandi – 9406090595
Follow for regular updates:
Website www.phmindia.org www.aipsn.net
Twitter @jsa_india
Facebook @janswasthyaabhiyan