08 JSA advisory on health systems preparedness Apr 2 v1
From Jan Swasthya Abhiyan (JSA) April 2, 2020
&
All India Peoples Science Network(AIPSN):
To
Secretary,
Department of Health & Family Welfare,
Govt of India, Nirman Bhavan,
Dear Sir/Madam:
Subject: Advisory to State and Central Governments
On strengthening health systems to manage the COVID 19 pandemic
Please find enclosed a detailed note prepared in a participatory and consultative manner by a number of organizations and concerned citizens who are part of our network of civil society organizations and peoples movements
We note that the country is going through a lock-down which has brought immense hardships to the majority of the people. The only justification for such suffering is to give time to the health systems to prepare for the oncoming epidemic. We have noted the significant number of measures that government has announced to step up the supply of testing kits, and PPE and ventilators, but we are worried that it would be little and late.
From our interaction at state level, we are deeply concerned that the preparations are patchy, slow, and selective. In our enclosed advisory, we have put together the very many aspects on which all state governments and the state governments needs to take immediate action. We demand that urgent action be taken on each and every one of these suggestions. We also call on you to include representatives of our organizations in monitoring the pace and comprehensiveness and quality of preparation.
We are also releasing this statement to the media so that they can also be informed on what, in our view, requires to be done. This would promote early identification of gaps and this would strengthen the effort at preparation.
We are also issuing an advisory to people and communities on what they require to do to protect themselves and to be of assistance to frontline staff of the department and all others who are working in partnership to help combat this epidemic. We would also be working to ensure social solidarity in this time of crisis.
T.Sundararaman
Sulakshana Nandi
N. Sarojini
D. Raghunandan
On behalf of JSA and AIPSN
Advisory to State and Central Governments
On strengthening health systems to manage the COVID 19 pandemic
INTRODUCTION:
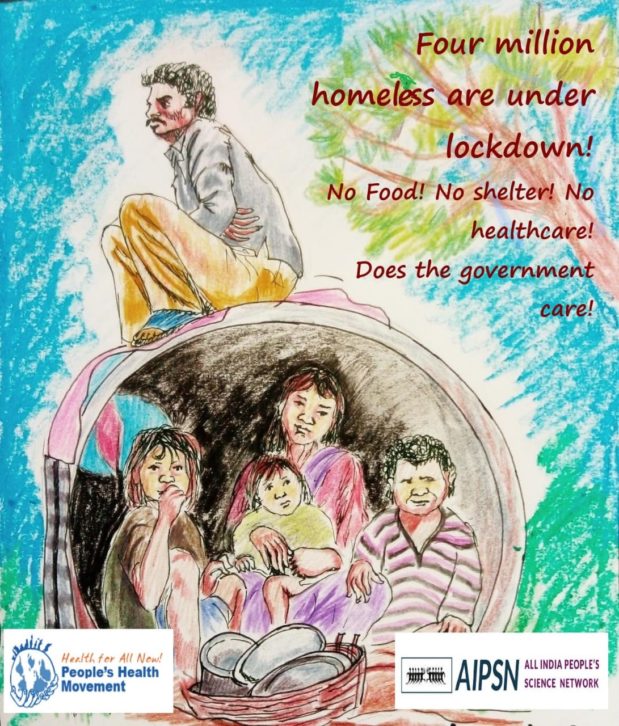
The lockdown implemented across the country only buys the government time to prepare the health systems for the coming epidemic. As, informal workers and poor people are paying an immense price in terms of suffering and even deaths; the urgency and moral obligation to prepare each state’s health system is even more.
We in people’s health movements, people’s science movements and in all movements of working people are seriously concerned by the lack of clarity on what is required in terms of preparation. Different state governments are prioritizing one or another aspects, failing to address the rest. We therefore call on governments to take immediate note of all the elements of preparing health systems that we list below:
These are based on the March 25th, 2020, briefing of the Director General of World Health Organization:
“ We call on all countries who have introduced so-called “lockdown” measures to use this time to attack the virus. You have created a second window of opportunity. The question is, how will you use it?»
The six key actions that we recommend are:
- First, expand, train and deploy health care and public health workforce;
- Second, implement a system to find every suspected case at community level
- Third, ramp up the production, capacity and availability of testing;
- Fourth, identify, adapt and equip facilities to manage risk, treat and isolate patients;
- Fifth, develop a clear plan and process to quarantine contacts;
- And sixth, refocus the whole of government on suppressing and controlling COVID-19.
These measures are the best way to suppress and stop transmission, so that when restrictions are lifted, the virus doesn’t resurge. The last thing any country needs is to open schools and businesses, only to be forced to close them again because of a resurgence. Aggressive measures to find, isolate, test, treat and trace are not only the best and fastest way out of extreme social and economic restrictions – they’re also the best way to prevent them
The eight measures we set out before are what state governments must do in the immediate to achieve the above objectives:
- Arrangements for Testing
- Arrangements for Isolation and Treatment of Mild and Moderate cases
- Arrangements for Treatment of Severe Patients and for Critical Care
- Addressing Human Resource Requirements
- Addressing Human Resource Rights and Safety
- Ensuring Supply Chain Management
- Ensuring Ambulance and Patient Transport
- Engaging community Volunteers
- Arrangements for Testing:
- Expand testing protocols to include all patients where the health care provider thinks it to be a clinically suspect case of Covid-19, based on clear, scientific standard protocols. This is required for both public health planning and because everyone who tests positive must be isolated. This is central to control of the epidemic – now and in the future. Denying testing to those with mild symptoms is a failure to isolate the main sources of infection and any amount of physical distancing will not make up for this. We note that he rate of testing in India is very low at around 20 tests per million compared to about 7000 tests per million in South Korea[1]. Though India has much less resources, there is clear need for very rapid increase in the number of tests being done. The main reason for this is restricting testing to contacts, foreign travel, which means that by protocol we are excluding the majority of COVID-19 patients who are mild and asymptomatic. This is leading to a false complacency as well as many clusters of infection growing unnoticed. It is also leading to all healthcare providers, even those not addressing COVID19 specifically getting infected. It is also required to guide areas where case searches and preventive measures have to be intensified.
- To achieve the above, hospitals need to ensure designated collection centres of samples in every district or preferably in every block. Immediately identify and train the concerned personnel in using PPE and collecting samples properly.
- Consider small mobile teams with adequate training and appropriate PPE collecting test samples from home in symptomatic patients in response to a phone call to a designated number. This will reduce infection when they come by public transport to the facility, and reduce infection at the facility when they wait to be tested. One possibility that the government can explore with due precautions is to use a number of volunteers who have recovered from the disease and therefore immune. To be safe they should have been tested to ensure that they are positive for antibodies and negative for the virus. Where distances are very big, and public transport very crowded this may be the only option.
- All testing must be free. All test results should be uploaded to an open repository with due care taken for privacy considerations. This will ensure that the test results can be checked publicly. A number that is linked to them could identify patients. So repeat testing can be followed up. Charges are to be considered only if the patient has come out of own accord with a doctor’s prescription for the test. Even that can be allowed only when the availability of test kits becomes much better than it is now.
- The testing protocol should ensure that all suspect mild moderate and severe cases are tested, and the necessary testing kits, equipment and reagents for this should be available. Asymptomatic contacts of COVID19 patients should also be tested on the 5th and the 14th day of the contact- but this could be included only when necessary test kits to test the symptomatic patients are in place..
- For the purposes of surveillance all these testing results should be anonymized, aggregated and reported to a central and state authority. In addition carefully selected surveillance sites should test a well drawn sample of the entire population to monitor true infection and case fatality rates, as well as the development of immunity. Antibody tests which are available would also be essential to test for asymptomatic infection and herd immunity.
2) Preparing for the Management of Mild and Moderate Cases
- In many nations there is an effort to hospitalize all mild and moderate cases so as to ensure good quality of isolation. Considering the large numbers that will be involved, private nursing homes, hostels and hotels will require to the requisitioned to serve as isolation hospitals. These are «hospitals» from the perspective that their occupants are sick persons, requiring a basic level of care that nurses and paramedics could provide. However some supervision by medical staff is required to identify those turning severe and referring them early.
- District administration should therefore earmark and prioritize the order in which beds would be requisitioned and deployed – for the first 100 patients, and then in further increments of 100. We note that there are plans to convert railway passenger trains into isolation center. Though as a desperate measure this may be a good idea, the average period of isolation would be anywhere from 10 to 14 days- and a railway compartment would be very restrictive. The recruitment of sports facilities and hostels and guest homes and hotels would be preferable.
- In districts where the public and private sector capacity to do this is weak, some of these centers could be managed by civil society organizations or local community based organizations or local self-government institutions- like municipalities and panchayat. These are then community managed institutional isolation sites with largely supportive care- food, water, symptomatic medicines, being organized and isolation being enforced.
- In all the above situations the working staff, should have adequate PPE.
- In many nations in the world even this has not been possible and home isolation has been resorted to. This is easier in middle class and privileged populations where housing has the necessary space. But in all circumstances it would require to be backed by good outreach services and monitoring.
- There should be a helpline in every state where people with symptoms can approach and be guided for whether to test, where to test, and transport for testing and/or isolation.
- The current approach of de facto denying the very existence of mild and moderate cases through a calculated strategy of non-testing and inaction will drive the epidemic forward.
3) Management of Severe Cases and those requiring Critical care and ventilatory assistance:
- For severe cases with signs of pneumonia confirmed by X-rays, hospitalisation should be ensured. Dedicated wards in existing health facilities should be utilised for this. In all such wards oxygen should be available, isolation should be possible and working staff should have PPE. Oxygen concentrators and pulse oximeters and consumables as required for acute respiratory illness with respiratory distress would also be needed in adequate numbers. Managing oxygen supplies is often a critical bottle-neck and this must be attended to.
- For critical cases, given the high requirement in skills, equipment, PPE and isolation it would be preferable to centralize management of severe and critical care patients in a dedicated COVID-19 hospital. Either requisitioning or recruiting a private sector hospital, or using a public hospital should achieve this. The existing caseload in that hospital should not be left without alternative. This is a reason why, in many states, a large under-utilized private hospital would be best commandeered. In many nations, entire hospitals have been built at short notice. This is may be required in some of the northern states where both public and private infrastructure is most inadequate.
- When planning for critical care and ventilators, we suggest a norm of one such bed and ventilator for about 30,000 population. However the requirement may increase if there is a surge (the curve did not get flattened) or where a big cluster of cases got established. It would decrease if there is higher mortality rate (about 90% of those on ventilators dying within two or three days) and increase if survival is better (patients may need 10 to 20 days of ventilator support). Sharing of such ventilators is possible to a limited extent. Efforts should be made to prevent the spreading out of ventilators across multiple hospitals. Ventilation in this disease requires a much more sophisticated equipment and a higher level of training. Ventilators should be pooled in one or two hospitals identified as nodal hospitals to treat COVID 19 patients. In cases where ventilation is required, we caution that any ventilator will not do.
- For the overall management of all COVID 19 patients in a district or a cluster of small districts, there should be one medical command centre for ensuring the preparation and allocation of resources, creating the necessary beds at different levels of care and allocation of patients accordingly. Proper guidelines should be set in place to prevent nosocomial or hospital-acquired infections. Care should be taken to ensure the separation of COVID-19 cases from routine patients in all health facilities.
- The orders required for requisition of private hospitals and nursing homes for isolation and treatment when the need arises should be issued now. Clear guidelines on costing, administration and treatment protocols should be laid out and finalized as soon as possible and before a crisis situation emerges.
- All treatment should be free. A few private hospitals that are undertaking COVID-19 care on their own, can be permitted to do so but treatment fees should be capped.
4) Human Resources for Combatting the Epidemic:
- To close the gap in human resources – the first and most immediate measure is to immediately fill existing vacancies by employing those who have applied for employment and are waiting at different stages of recruitment. Online interviews and video conferencing, as done in Kerala, is a feasible option. Those employed on short-term contracts and contracted through third party agencies are at risk of discrimination with regard to access to personal protective equipment, leave and other safeguards. Additional care has to be taken to ensure that they are involved and/or covered by all the necessary procedures.
- Put in place on-line training programs on COVID 19 for the entire medical workforce in the country, facility based training for the entire workforce in the each facility, including ASHA and community-based health workers attached to different health posts.
- The medical professional at the nodal hospitals should be given training to manage ventilators in case of Acute Respiratory Distress Syndrome (ARDS) arising out of COVID 19 infection. Web-based training is a start- but on the job mentoring by experienced domain expertise would be required.
- The entire staff in all COVID-19 earmarked hospitals, ICU units and isolation centers should have proper training and this should include both guidelines and protocols for COVID-19 care, as all as personal safety, infection risk management and the use of personal protective equipment. The government should provide guidelines for these procedures to be followed in private facilities.
- For work such as contact tracing, outreach support to those in home quarantine or isolation, develop a policy of health care auxiliary workers- not only ASHAs, but also including volunteers.
- States should ensure that the logistics to supply equipment and material for hospitals and health centres is not hampered due to the lockdown.
5) Ensure health workers rights and safety
- The rights of all health workers should be protected. Wages should be provided as per existing government norms, and extra hours remunerated as per the law. Considering that health workforce in private facilities will also be involved in responding to the epidemic, and facing higher risks that what health workers face in their usual settings, state governments should ensure compliance with the Supreme Court Recommendation related to wages in private healthcare facilities In many situations a special risk allowance could be considered. Special paid leave in case of Covid-19 related sickness and quarantine should be provided, including to workers on short-term contracts and employed through a third party.
- Health workers undergo considerable stress during this period. Therefore counseling and mental health support should be made available. Breaks and time-off should be maintained, as healthcare workers’ burnout aids spread of virus. Health workers displaying Covid-19 like symptoms should not be asked to continue attending to work. Health workers’ right to opt out of work when they are not provided with a safe working environment and adequate protective equipment should be respected. Health workers working in high risk areas, such as isolation wards, have to be provided the option of adequate hostel accommodation so that they can avoid going home where there are old relatives or young children whose health they are concerned about.
- For health worker safety adequate availability and training to use the necessary Personal Protective Equipment (PPE) is essential. These guidelines should be clearly displayed and followed. Those who refuse to work because of violation of these guidelines should not be penalized. These guidelines should apply and their implementation monitored in private health facilities too A monitoring system should be put in place so that health workers can raise concerns about violation of guidelines and action taken accordingly by the relevant government.
- Maintenance of and adequate supply chain for PPEs and safety equipment for health workers is one of the key challenges before governments and they should be held accountable for this. Government of India should examine the feasibility of its rigid criteria for PPEs and adopt the more practical, yet adequate, WHO guidance on the same. The inability to follow unnecessarily
demanding guidelines should not become an excuse to avoid strict implementation of the WHO guidance (see PHM Advisory in this regard). - Training should be given on infection risk management and on how to use PPEs. All health workers should be provided with communication materials on the use of PPEs. Guidelines should clearly mention as to who are at what level of risk and the adequate PPE requirement for different workers. The government should engage with trade unions of health workers to ensure that the guidelines effectively reach = all concerned health workers. Facility management should facilitate an active role of health workers’ representatives in determining safety measures and safeguards of their health.
- Free access to health care for health workers dealing with the Covid-19 outbreak, even in events that do not lead to hospitalization, has to be ensured for all health workers, including those working in facilities under the central and state government, but also municipal and local bodies, in the private sector, and health workers with informal employment conditions.
6) Supply Chain Management:
- The pandemic management is going to require a very high degree of efficiency and time-lines and quality controls to ensure that the necessary testing kits, medicines, and PPE are available where they are needed, when they are needed, and in adequate quantity and quality.
- States like Tamil Nadu, Rajasthan and Kerala have already robust systems in place for doing this, but even they would find it difficult. States, which have not established such systems, must immediately put together a state level authority, which can manage this using the guidelines from the exemplar states. In consultation with center, where the funds are from the center, procurement procedures must be simplified to meet the situation.
- Given that manufacturing capacity is the key bottleneck, both states and center should set up task forces which will look at the choice between manufacturing within the state and/or purchasing from outside, make forecasts of the requirement, identify and address potential barriers and then place orders well ahead of the peak of the epidemic. The center has to ensure that patent and trade barriers do not come in the way.
- Ambulances and Patient Transport:
- There would be the need to designate some ambulances with advanced life support for shifting patients in need of ventilation and many other patient transport vehicles for shifting patients suspected of COVID 19 for testing, or of confirmed cases for hospitalization, isolation etc.
- The number of ALS ambulances and patient transport vehicles required would vary with the surge and clustering of cases. Norms can be developed. In states where the number of public ambulances under the 108 and related services is well below requirements, order for more ambulances should be placed NOW.
- Mechanisms for sterilization of the ambulances, training and low risk PPE for drivers and training with high risk PPE for accompanying emergency technicians, should also be put in place.
8) Community Volunteers and Community Participation.
- Ensuring community participation is essential. We will need volunteers to do surveillance and tracing. These volunteers can be enrolled from within the community or through community based organizations.
- People who are discharged after COVID-19 treatment can be a useful resource and they should be encouraged to volunteer. They will be able to help in home isolation and their experience of encountering the disease will help in changing the perspective around it. They would also help in tasks like institutional isolation, home and institutional quarantine, contact tracing. Some of them, especially if from within the health workforce could be useful for testing.
- The availability of antibody testing for past infection and immune status is expected to become available. Given the way we have managed mild and moderate cases, this “individuals who have recovered from infection” may be useful asset as community volunteers.
- Community Organizations would need to be deployed widely for many tasks including relief and welfare measures to reach most the vulnerable sections, management of home and institutional quarantine, monitoring of human rights issues, campaigns against stigmatization of the disease and public education, as required.
In conclusion:
The State and district level units of peoples health movements and peoples science movements and of a wide variety of civil society organizations and trade unions and workers associations stand ready to help the government and communities in combatting this pandemic and the humanitarian crisis that both the pandemic and measures to contain it have led to. The government must make use of this resource.